By Siha Hoque
Hormones are essential in regulating our every bodily function, and we have over 50 different major types present in our systems. One of these hormones is aldosterone, and its role in the body is to control our blood pressure and volume.
Aldosterone, secreted by the adrenal glands, raises blood pressure by signalling to the kidneys to increase the reabsorption of sodium into the bloodstream, in order to increase blood volume, therefore pressure. It can also increase the amount of potassium being secreted into the urine, which reduces its concentration in the blood. Both these signals and changes to the electrolyte concentrations in the blood can help to increase blood pressure after a decrease has been detected.

See above: Aldosterone's chemical structure.

See above: Location of adrenal glands.
A surplus of aldosterone however, as seen in Primary Aldosteronism, can have very negative impacts for the body, as it leads to problems including hypertension (high blood pressure) and low potassium levels in the blood, or hypokalemia. This is particularly dangerous, as when advanced, it can increase the risks of heart and/or kidney failure.
Primary Aldosteronism can be treated by surgeries to remove tumours on the adrenal glands if that is the cause of the disease, or removal of one of the glands if it is solely responsible for overproduction, however if not either of the above, aldosterone blockers such as spironolactone can be taken instead. If left without treatment for too long, heart arrhythmia can set in, and damage to blood vessels can accumulate, such as thickening and ageing of the vessel tissues.
Consequently, it is important for the imbalance to be recognised early. The standard diagnostic techniques are to take a blood sample from the patient after they have completed light physical activity and analyze to see if abnormal levels of aldosterone are present. This is usually followed by confirmation testing to see if aldosterone levels reduce with a high sodium intake (this would lower the blood pressure of an individual by increasing the blood volume) and if no change occurs, further screening to find the source of high aldosterone production. This could be a CT scan to identify if nodules have developed on the glands - however this isn't always the cause of the condition. Alternatively, a more accurate confirmation is to take samples directly from adrenal veins - Adrenous Venous Sampling/AVS - to see if either or both sides are overproducing, however this is an invasive and often intense procedure for patients.
As of 2025, this diagnostic method has been viewed by medical experts as outdated and flawed, with under 1% of people suffering from Primary Aldosteronism correctly diagnosed.
Recently, a new imaging technique for this condition has been developed at University College London, and it has proven to be more accurate and less invasive - PET-CT scans can detect and show the hyperactivity of one or both of the adrenal glands in Primary Aldosteronism (something which is invisible in other scans) on a detailed 3D image. This reduces the time taken for a diagnosis to be made, reduces hypertension-driven risks to a patient's health and the accumulation of the damage to the body from this condition.
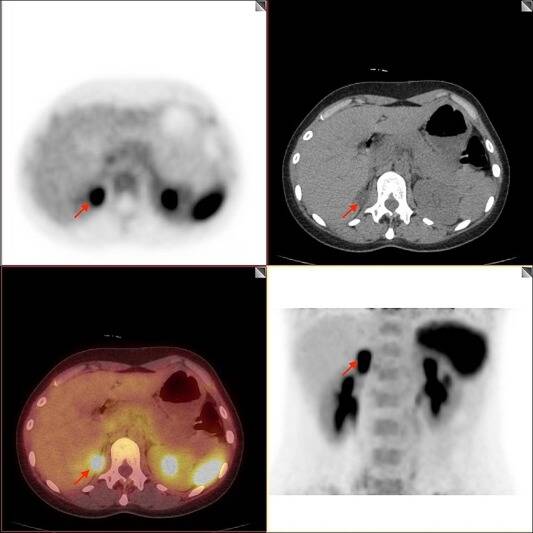
See above: PET-CT Scans showing Primary Aldosteronism.

See above: A CT Scanner.
A CT scan, or computed tomography, is often used in medical treatments, often to find tumours and blood clots. It works by sending X-rays into the body from various angles, where they are then detected and sent to computers, where cross-sectional images from these X-rays can be formed to give a detailed view of various structures in the body. CT scanning was a Nobel Prize-winning development, invented by Godfrey Hounsfield and James Ambrose in October 1971, and has been in use for around 50 years.
Only a few years after this, the first human PET scanner (Positron Emission Tomography) was invented by Micheal Phelps and Edward Hoffman at Washington University. PET scans work by measuring the metabolic activity of different cells within the body. A tiny amount of a radioactive tracer is used in PET scanning, and can be injected into the body, where it is absorbed by cells. Cells with high metabolic activity absorb more of this radioactive tracer, and this can therefore highlight tissues which have very high levels of metabolic activity, such as the uncontrolled cell division and tissue growth of cancer cells in tumours. The radioactive substance decays not long after its absorption, and emits positrons, which collide with the electrons to produce gamma rays. The PET scanner can detect these gamma rays and pinpoint the location which they came from, therefore the location of high metabolic activity, and create a 3D image showing where the tracer has accumulated.

See above: A patient getting a PET Scan.
The two scans described above can be combined into a PET-CT scanner, where the radioactive tracer detecting high cell activity and the detailed 3D X-Ray images can be combined to show specialists the structure and performance of the body. In the case of Primary Aldosteronism, this new diagnostic technique is not only far less invasive, but due to its high accuracy and speed, shows promise for solving the problem of under-diagnosis and ensuring patients can receive the correct treatment sooner.


Add comment
Comments