By Nina Mohamed
High blood pressure or hypertension is often referred to as a “silent killer" by many physicians as it is known for not presenting any symptoms until significant damage is done. This condition affects over 30% of the world's population, according to the Pan American Health Organisation, and is a major risk factor for a variety of serious health issues such as heart failure, kidney disease, and vision loss. Given its widespread impact and insidious nature, understanding its origins is the crucial first step toward effective management.
The roots of hypertension are often complex, generally dividing the condition into two main categories: primary and secondary. Primary, or Essential, Hypertension accounts for the vast majority of cases, typically developing gradually over many years. For this type, there isn't a single, identifiable cause; rather, it’s a confluence of factors, making both lifestyle and genetics key players. Significant risk factors include age, as arteries naturally stiffen over time, a family history of hypertension, and underlying chronic conditions like Type 2 diabetes. However, our daily habits play an undeniable and massive role, with factors such as a diet high in sodium (salt) and low in potassium, a chronic lack of physical activity, excessive alcohol consumption, and unmanaged, persistent stress all being significant contributors that put constant strain on the cardiovascular system.
In contrast to the gradual development of the primary type, Secondary Hypertension is caused by an underlying medical condition, often appearing suddenly and resulting in higher blood pressure. Conditions that can trigger this type include various forms of kidney disease, problems with the adrenal glands, which produce hormones that regulate blood pressure, and certain congenital heart defects. The key difference here is that treating the underlying condition can often be enough to bring the blood pressure back into a healthy range, offering a more direct path to relief than the multifaceted approach needed for primary hypertension.
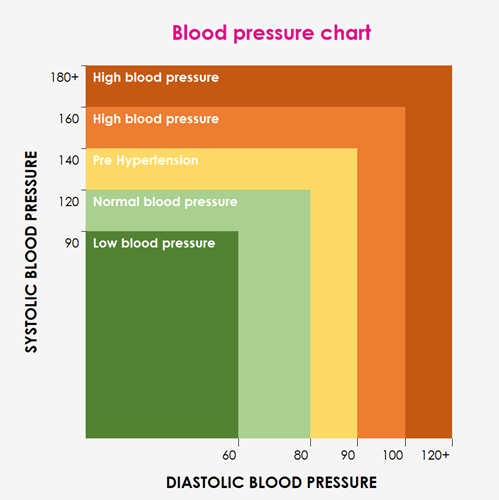
Because hypertension rarely gives warning signs, regular screening is the only reliable way to catch this condition before it causes severe organ damage, a necessary vigilance due to its silent nature. Diagnosis is made by a healthcare provider using a standard blood pressure cuff (sphygmomanometer) to measure the pressure in your arteries, providing two values: systolic pressure, the top number measuring the pressure when your heart beats, and diastolic pressure, the bottom number that measures the pressure when your heart rests between beats. According to current medical guidelines, a reading of 130/80 mm Hg or higher is typically considered in the hypertensive range.
However, a diagnosis is rarely made based on a single reading because blood pressure naturally fluctuates based on temporary factors like stress, recent activity, or caffeine intake. For this reason, your doctor will usually take several readings over a series of visits to confirm a pattern of sustained elevation. Some patients experience “white-coat hypertension,” where their blood pressure is temporarily elevated only in a clinical setting due to anxiety. In such cases, your doctor may recommend ambulatory monitoring, which involves wearing a portable device that measures blood pressure at regular intervals throughout the day and night to get a true picture of your average pressure outside of the clinic. Confirming this sustained pressure elevation is vital because the danger of the "silent killer" lies in the fact that every hour your blood pressure remains high, it silently damages your body’s delicate network of blood vessels and vital organs.
The constant, excessive force weakens and stiffens the arteries, leading to a host of debilitating, life-threatening complications, starting with the heart itself. Hypertension is the leading risk factor for heart attack and stroke because the heart has to pump harder against the high resistance, which can lead to a thickening of the heart muscle, eventually causing heart failure. Furthermore, the damaged arteries are prone to the build-up of fatty plaques (atherosclerosis), which increases the risk of a coronary blockage. This vascular damage extends into the brain, where weakened blood vessels can either rupture, causing a hemorrhagic stroke, or become blocked by a clot, causing an ischemic stroke, both of which lead to brain damage, disability, or death.
Beyond the heart and brain, the body's delicate filtering systems are also extremely vulnerable, particularly the kidneys. These organs rely on a vast network of tiny, fine blood vessels, and high blood pressure can damage them, impairing the kidney's ability to filter waste and excess fluid from the blood. Over time, this damage can progress to kidney failure, requiring dialysis or a transplant. Finally, the eyes contain similar extremely small, delicate blood vessels, and hypertension can damage the blood supply to the retina (hypertensive retinopathy), potentially leading to blurred vision or permanent blindness. Recognizing these grave risks makes the commitment to management all the more urgent.
The good news is that hypertension is one of the most manageable chronic conditions, and treatment focuses on a comprehensive, two-pronged approach: therapeutic lifestyle changes and, when necessary, medication. For many people, making significant lifestyle adjustments can be enough to bring blood pressure into a healthy range or significantly reduce the need for high doses of medication. These powerful changes include adopting the DASH (Dietary Approaches to Stop Hypertension) diet, which is highly effective and involves reducing sodium intake, increasing potassium-rich foods, and prioritizing whole grains, fruits, vegetables, and lean protein.
Equally vital to success is aiming for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, swimming, or cycling, as physical activity strengthens the heart and makes arteries more flexible. Furthermore, losing even a small amount of weight, just 3 to 6 kg, can meaningfully lower blood pressure, and eliminating or severely limiting alcohol and smoking is one of the most powerful steps you can take, as both severely constrict blood vessels. When lifestyle modifications are insufficient, a physician will prescribe antihypertensive medications, which can include a variety of drug classes designed to work on different mechanisms, such as diuretics, ACE inhibitors, ARBs, or calcium channel blockers. Often, a combination of these drugs is used to achieve the optimal target blood pressure. Successfully managing hypertension requires consistent monitoring and a strong partnership with your healthcare provider; by committing to these changes and treatments, individuals can protect their vital organs, maintain their quality of life, and dramatically reduce the risk of falling victim to the “silent killer.”


Add comment
Comments